HeartFailureeducationforMDandnurse060209.docx
《HeartFailureeducationforMDandnurse060209.docx》由会员分享,可在线阅读,更多相关《HeartFailureeducationforMDandnurse060209.docx(17页珍藏版)》请在冰豆网上搜索。
HeartFailureeducationforMDandnurse060209
DanSorescu,MD,updatedJune2,2009
HeartFailureEducationforMDsandNurses
Apracticalguideforinpatientmanagementofpatientsadmittedfor
Acutelydecompensatedheartfailure(ADHF)
EmoryUniversityMidtownHospital
PartA:
CarefortheHospitalizedPatientwithHeartFailure
Whatnursesandphysicianneedtoknowforagoodpatientcareoutcome…
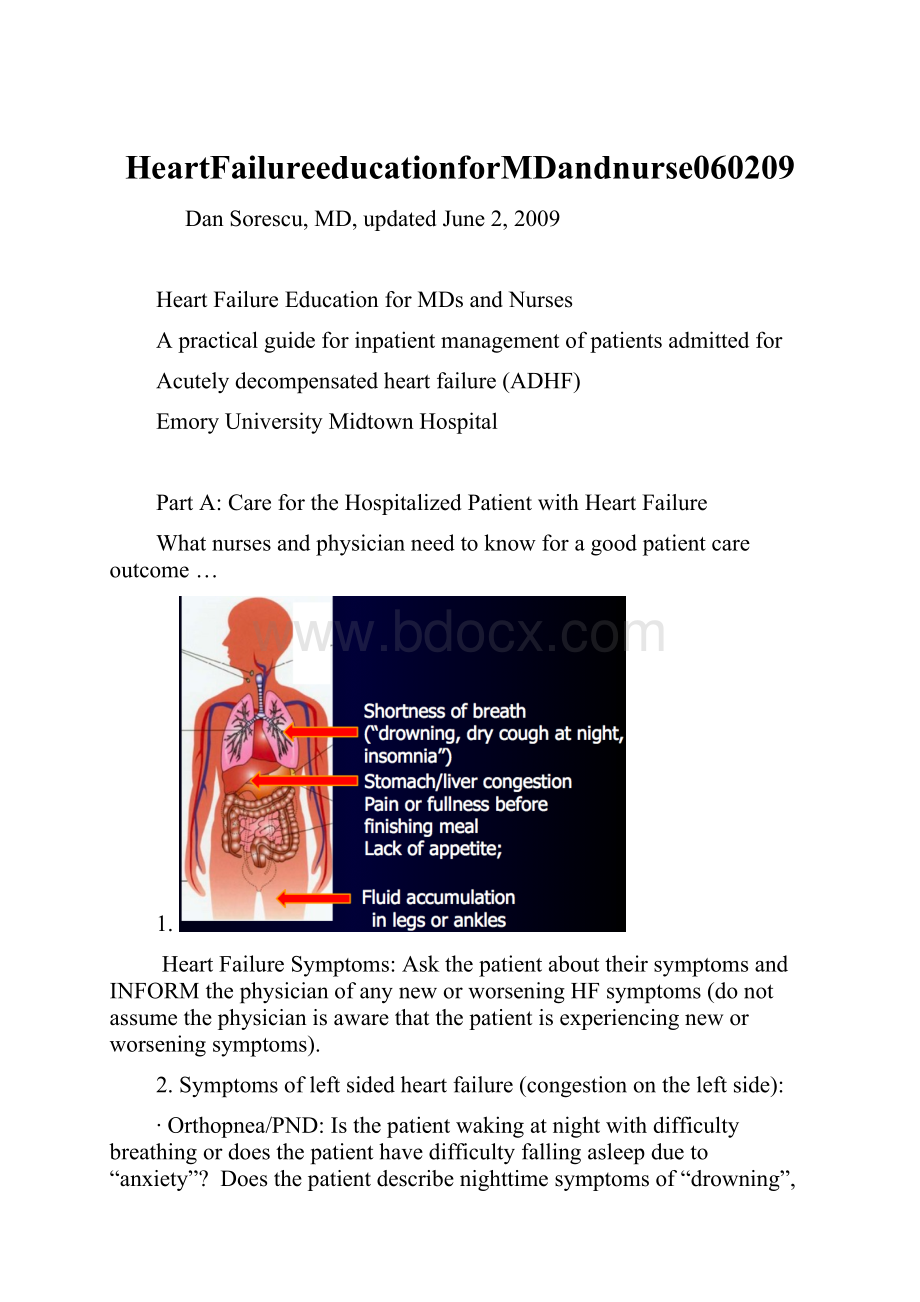
1.
HeartFailureSymptoms:
AskthepatientabouttheirsymptomsandINFORMthephysicianofanyneworworseningHFsymptoms(donotassumethephysicianisawarethatthepatientisexperiencingneworworseningsymptoms).
2.Symptomsofleftsidedheartfailure(congestionontheleftside):
∙Orthopnea/PND:
Isthepatientwakingatnightwithdifficultybreathingordoesthepatienthavedifficultyfallingasleepdueto“anxiety”?
Doesthepatientdescribenighttimesymptomsof“drowning”,“smothering”,insomnia,orhavingadrycoughatnight?
Thesec/o’sareoftentimesequivalentsymptomsforparoxysmalnocturnaldyspnea(PND)duetoshiftofwaterfromperipherytolungsatnight.
∙DOE:
Isthepatientexperiencingworseningdyspneaonexertion(DOE)andifso,whendiditstart?
Isthepatientexperiencingworseningexercisetolerance(feelingmoretiredorfatiguedwithanyactivity)—whenwasthisworseningexercisetolerancefirstnoticed?
Worseningexercisetolerance(DOE)mayindicateworseningcardiacoutputandheartfunction.
∙OrthostaticDizziness:
Doespatientreportdizzinesswheninverticalposition?
Orthostaticdizzinesssuggestsintravasculardepletionfromoverdiuresis,sepsisorverylowcardiacoutput.
3.Symptomsofrightsidedheartfailure(congestionontherightside):
∙Poorappetite,earlysatiety:
Ispatientexperiencingaworseningofappetite?
Assessifthepatientcaneatacompletemealwithoutfeelingfullornauseated.
∙Payattentionifthepatientishavingepigastricpainorfullnessbeforefinishingamealandwhichisclearlyaggravatedbymealsassociatedwithanincreaseintheirabdominalgirth(ascites).Theabovesymptomsareoftenduetoliverandstomachcongestionfromheartfailure.Thesesymptomsareespeciallypresentinpatientswithadvancedheartfailurewhorequirechronicdiureticuse.Donotbefooledifthereisminimalevidenceofperipheraledemainpresenceofrightsidedheartfailurewithvolumeoverload.
∙Decreasedurineoutput:
Payattentiontotheeffectivenessofthediureticregimen.Aretheyhavingthesameeffectaswheninitiallydosed(causingsimilaramountofurineoutputasbefore)?
Whenthereisstomachandlivercongestion,medicationabsorbtiondecreases,especiallyforfurosemideandhydralazineandreducestheireffectivenessandpatientswillcomplaintheydon’tworkanymore.
∙LowerextremityEdema(LEE):
Anylowerextremityswelling?
Inordertoquantifyedemaseebelow.
4.Importantinformationaboutthepatient’soutpatientHFcarepriortoadmission:
∙Whoisthephysicianwhomanagestheirheartfailure;whenwaslasttimetheysawhim/her?
∙Whoistheir“helper”orcoachathome?
Studieshaveshownthatpatientswhohaveacoachathometohelpimplementthetherapyanddietaryinstructionsdomuchbetterthantheoneswhodon’t.Ifthepatientdoesnothavea“helper”or“coach”,whoistheirmainsupportandisthispersonabletoprovidesupportatthistime?
∙HomeMedicationspriortoadmission?
Aretheytakingthemroutinely?
∙WhenwaspatientfirstdiagnosedwithHFandhowfrequentlydotheyrequirehospitalizations/ERvisits?
AretherebarrierstoHFtreatments(financial,social,perceptionofillness,cognitiveimpairment)?
∙Saltrestriction(dotheyeatout,etc),dotheyknowhowtoreadlabels?
∙PriorTests/Therapies:
Didtheyhavearecentstresstest,cardiaccatheterization,pacemaker/defibrillatorandifsowhenwaslasttimetheyreceivedashock.Whoisfollowingtheirpacemaker/ICDandwhattypeofdevicedotheyhave(Medtronic,etc).
5.Otherillnesses(co-morbiddisorders)thatcandecompensateheartfailureandaffect/complicateitstreatmentinhospital:
∙Anysignsofinfection(URI,UTI,etc).
∙Anyjointaches,swelling?
(GOUTattackswhichalwaysoccur1-2weeksafterarecentincreaseindiureticsuse).
oEitherinflammation(gout)orinfectionswillcauseinappropriatevasodilatationofperipherywithvasoconstrictioninthekidneys,whichwilldecompensatetheirheartfailureandoftenuspreventfromtreatingit(needtoholddiureticsandvasodilatorsuntilUTI/goutresolves).
∙Anydiarrhea(causeslostofKandMgandtriggersarrhythmiasandshocksfromICD)orconstipation(alterstheabsorbtionofvitaminKandthereforeresponsetowarfarin).
∙Headache(mostcommonsideeffectfromnitrates)anddizziness(mostcommonsideeffectfromhydralazine).
6.Physicalexamofthepatientadmittedwithacutelydecompensatedheartfailure(ADHF):
VitalSigns
oIdeally,everypatientadmittedwithADHFshouldhaveorthostaticBPandpulseperformed/documentedonadmission.Iforthostatichypotensionispresent,thepatientlikelyhasintravasculardepletionorissepticandoftenrequireswithholdingofdiuretics.
oDocumentsystolic,diastolicandmeanarterialpressure(MAP).Note:
AnidealMAPis65-70mmHg(thiscorrespondstoanSVRof900-1000)inthosepatientsadmittedwithacuteCHF.Thepulsepressure(PP)isdifferencebetweensystolicanddiastolicBPdividedbysystolicBP.
oSBPreflectsmorethestrokevolumeandthereforecardiacoutputandwilldecreaseascardiacoutputdiminishes.Typically,eveninpriorhypertensivepatients,thesystolicBPwillgodowninadvancedheartfailurebecauseoflowEF.ForexampleaBPof110/90isactuallyseverehypertensionforthesepatientsbecausehighMAPreflectssevereperipheralvasoconstriction(iftheyhadnormalEF,SBPwould’vebeen200mmHg!
)andthisisofteninterpretedwronglybyMDsashypotensionandleadtoinappropriatewithholdingofvasodilators!
Oftenthesepatientswillbecomehypertensiveagainoutpatient,2-3monthsaftertheyareplacedonappropriatedrugstoimprovetheirEF.
oDBPreflectsmoretheperipheralvasculartoneandwillincreasewithvasoconstriction(highsystemicvascularresistance(SVR))andwilldecreasewithvasodilatation(highSVR).Therefore,asmallPPequalslowcardiacoutputwhileahighPPequalsnormalorhighcardiacoutputwhichstronglysuggestssystemicinflammation(gout)orsepsis(UTI,etc).Anydiastolic>70mmHgisabnormalhighinpatientswithADHF(patientisvasoconstrictedandneedsvasodilators),thesameanydiastolic<50mmHgisinappropriatelow(patientistoovasodilatedandmayhaveSIRSorsepsisandmayneedpressors).
∙IftheMAPis>70mmHg;thisisinappropriatelyhighforapatientwithacutelydecompensateheartfailureandvolumeoverload.
∙Ifthepatientiscold(vasoconstricted)andwet(edema,volumeoverload)
oA)Ifthepulsepressureisnormal(SBP-DBP>25%ofSBPbutlessthen50%),thenpatientneedsvasodilatorsfirst(tovasodilateandincreasecardiacoutput)andthendiuretics.
oB)Ifthepulsepressureislow(PP<25%ofSBP,example90/70mmHg),thenpatienthaslowstrokevolume,treatmentisthesamebutthepatientmayalsobenefitfrominotropes(milrinoneordobutamine).IngeneralthereisnoneedforinotropesaslongasMAP>70mmHgandpatienthasgoodrenalfunction.Howeverifrenalfunctionworsens(renalhypoperfusionduetolowcardiacoutputandrenalvasoconstriction)andpatientisstillsymptomaticwithcongestion(stillneedsdiuretics)thenmaybenefitfromadding/switchingtoaninotropbeforeadministeringdiuretics.
∙IftheMAPis<65mmHg.
∙A)Andthepatientiswarmandwet,withpulsepressure>50%(exampleBP90/40mmHg)thereismostlikelyconcomitantsepsis(UTI,etc)orotherinflammatoryexplanation(suchasgoutorSIRS=systemicinflammatoryresponsesyndrome)whichinappropriatelyvasodilatestheperiphery(lowSVR)andvasoconstrictsthekidneyoftenwithworseningrenalfunction.Thevasodilatorsanddiureticsneedtobewithholdbecausewillaggravaterenalfunction.Oncontrary,oneneedstoincreaseMAPto65-70mmHgtoshiftthebloodbackfromperipherytomainorganstoimprovetheirperfusion.Occasionally,patientneedtobetransferredtoICU/CCUtoreceivelowdosepressors(norepinephrine2-5mcg/min)toraisetheMAPandimproverenalperfusionwhilewearetreatingtheunderlyinginflammatory/septiccondition).
∙B)Andthepatientiswarmanddry,thencheckorthostaticstoconfirmthatpatientisintravasculardepleted.Thisconfirmstrueoverdiuresisandweneedtostopdiureticsandvasodilatorsandgive2litersofwater-ideallyorally.Ifpatientispersistenthypotensiveonemayrepletefluidwithiv500-1000mlof½NSover2-4hours(avoidNSwhichgivestomuchsaltandwillalwayscausenextdayinappropriatevolumeexpansionduetoexcessivesodiumloadandpatientrecurringCHF).
∙C)Andthepatientiscoldandwet-thenlikelypatienthasseverelyreducedcardiacoutputduetobothinappropriatevasoconstrictionandlowEF.Thetreatmentwillbetofirststartaninotrope(dobutamine5mcg/kg/min)andcheckagainBPin30min.Ifindeedthatisthecase,usuallytheMAPwillincrease>65mmHgandthenwecanalsoaddthevasodilators(again,weneedtodothisbeforegivingdiuretics).
∙D)Andthepatientiscoldanddry(liesflatwithoutbeingSOBandnoevidenceofperipheralandcentraledema),-patientmaybeintravasculardepletedfromoverdiuresisandmayneedinotropes(severelyreducedcardiacoutput).Ifthatisthecase,administrationof500mlof1/2NSover1hourshouldincreasetheMAP>65mmHg.IftheMAPisstilllessthen65mmHgthepatientneedsinotropestooandmayben